In addition, the catch-all term of carcinoid should only be applied to well-differentiated tumors with serotonin reactivity of a midgut origin. To top it all off, most carcinoid patients are asymptomatic.
It's no wonder that clinicians are searching for the best imaging modality to diagnose, differentiate, and treat endocrine tumors. Two recent studies looked at how molecular imaging and therapy fared in this disease. A group from Poland evaluated endocrine cancer response to treatment with a radiolabeled somatostatin analogue, while researchers in France tested two molecular imaging techniques in endocrine cancers as a tool for diagnosis and staging.
90Y DOTA TATE
In the first study, the Polish specialists evaluated the effect of treatment with 90Y DOTA TATE in endocrine tumors of the digestive tract (GEP-NET). This radioactive somatostatin analogue responds to the excessive expression of somatostatin receptors in malignant tumors, attaching itself to the neoplasm and destroying it.
Treatment with 90Y DOTA TATE "can eliminate the cancer cells using high energic ß-electron toxic to other normal tissue due to direct binding," explained Dr. Jaroslaw Cwikla and colleagues in a poster at the 2006 Society of Nuclear Medicine meeting in San Diego, CA.
Cwikla is from the nuclear medicine division at the Postgraduate Medical Center in Warsaw. His co-authors are from the Hospital Ministry of Internal Affairs and Administration, as well as the Maria Sklodowska-Curie Memorial Center, also in Warsaw.
 |
|
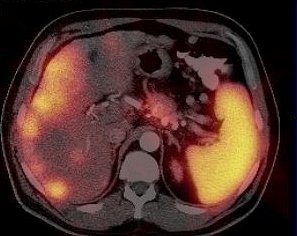
A 52-year-old patient with pancreatic non-secretor neuroedocrine carcinoma low malignancy (NECLM; foregut; WHO type 2). SPECT and CT scans before start of 90Y DOTA TATE treatment, fusion images of standard CT after IV contrast enhancement and SRS using 99mTc HYNIC TATE.
|
For this study, 19 patients with an established histological diagnosis of GEP-NET were treated with 90Y DOTA TATE. An objective response was measured using the response evaluation criteria in solid tumors (RECIST) guidelines (Journal of the National Cancer Institute, 2000 February 2, 2000, Vol. 92:3, pp. 205-216; European Journal of Cancer, May 2006, Vol. 42:8, pp. 1031-1019).
All patients received an average dose of 14.8 GBq in three to four therapy sessions over six to eight weeks. Anatomical response was assessed with CT as well as evaluation of clinical symptoms. Planar white blood cell scanning was used to confirm tumor uptake. Scans were judged based on partial response, complete response, disease stability, and disease progression using RECIST criteria.
According to the results, there was no significant toxicity or any adverse events during 65 90Y DOTA TATE sessions over a one-year period. Based on RECIST, 58% of the patients had disease stability, 26% had partial response (two cases of midgut tumor; three cases of foregut tumor), and 16% had disease progression (six midgut endocrine carcinoma of low malignancy; four foregut tumors; one malignant phenochromocytoma).
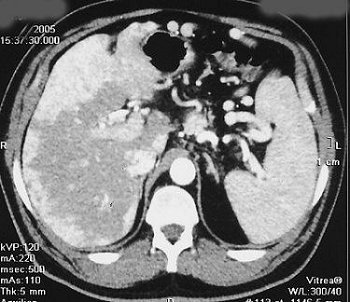 |
Same patient. Above, CT scan 12 weeks after the start of the radionuclide treatment. Below, CT scan done six weeks after completed therapy of 90Y DOTA TATE. RECIST = disease stability. Serum CgA increased. Patient was clinically well at six-month follow-up. Images courtesy of Dr. Jaroslaw Cwikla.
|
A biochemical response in the form of a significant drop of serum CgA was noted in 42% of the patients, while a clinical response was found in 63%. Only the patient with a malignant phenochromocytoma reported worsening pain and disease progression on CT.
The group concluded that more tumor-specific treatment was possible with 90Y DOTA TATE as evidenced by the significant clinical and biochemical response to treatment in their patient population.
PET versus SRS
In previous studies, Cwikla's group looked at the best diagnostic algorithm for imaging endocrine tumors. In a 2004 paper, they compared the value of CT and MRI when added to 111In-octreotide somatostatin reception scintigraphy (SRS). They found that individually, none of the modalities were that adept at disease evaluation, but that combining MR and SRS resulted in higher diagnostic value. In the second study, they suggested that CT and SRS could be used in conjunction, but that ultimately, pathology and immunohistochemistry results would be the key to patient management (Medical Science Monitor, June 2004, Vol. 10: supplement 3, pp. 9-16; Polish Journal of Radiology; September 6, 2005, Vol. 70:4, pp. 87-96).
In new study published this month, a multispecialty group from France has proposed using 18F-fluorodihydroxyphenylalanine (18F-FDOPA)-PET for the diagnosis and follow-up of digestive endocrine tumors. They also performed a head-to-head comparison of 18F-FDOPA-PET with 111In-pentetreotide SRS.
As with Cwikla's group, Dr. Françoise Montravers and colleagues stressed that precise tissue histologic characterization was very important in order to achieve complete morphologic imaging results. Nonetheless, this multispecialty group found that the PET paradigm offers useful information about the nature of digestive endocrine tumors, as well as some advantages over SRS.
"18F-FDOPA-PET is based on the capacity of endocrine tumor cells to take up, decarboxylate, and store amino acids," wrote Montravers, who is a nuclear medicine specialist at the Hôpital Tenon AP-HP and the Université Pierre et Marie Curie, both in Paris. Her co-authors are from the gastroenterology department at her institutions and the Hôpital Beaujon AP-HP in Clichy, France.
The authors pointed out that during the study period (2002-2005), 18F-FDOPA was not approved for use as a radiopharmaceutical in France (Journal of Nuclear Medicine, September 2006, Vol. 47:9, pp. 1445-1462).
The study population consisted of 30 consecutive patients with histologically proven malignant digestive endocrine tumors. Fifteen patients with known small-bowel carcinoid tumors; eight with non-carcinoid tumors; and seven with primary tumors underwent PET and SRS. The SRS exam was done first and the median time between the two exams was 20 days. PET scans were done with either 2 MBq/kg of 18F-FDOPA (C-PET, Philips Medical Systems, Andover, MA) or 5 MBq/kg of 18F-FDOPA (Gemini PET/CT, Philips Medical Systems).
|
|
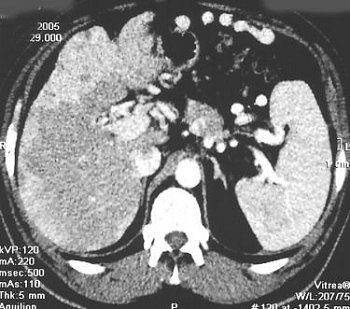
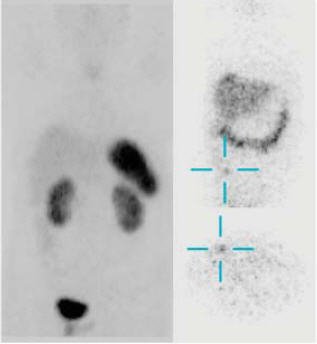
Search for primary tumor after detection of bilateral ovarian metastases of well-differentiated endocrine tumor. Bilateral ovariectomy was performed as part of radical surgery for uterine carcinoma. CT and contrast-enhanced bowel x-rays were negative. Primary tumor was clearly identified with 18F-FDOPA PET/CT. Copyright © 2006 by the Society of Nuclear Medicine.
|
Data were analyzed on a per-patient basis, and there were three possible endpoints to the study, with PET turning in results that were equal to, better than, or worse than SRS.
According to the per-patient analysis, the sensitivity of 18F-FDOPA-PET was 63% and the accuracy was 67% versus 78% sensitivity and 76% accuracy for SRS. 18F-FDOPA-PET was accurate in 17 of 19 exams with one false positive (FP) in a small-bowel carcinoid and one false negative (FN) in a small-bowel (3 mm) tumor. In non-carcinoid tumors, the PET studies were accurate in five of 14 exams.
|
|
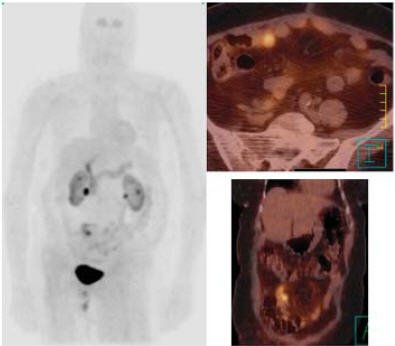
Same case as above. 111In-pentetreotide SRS provided a doubtful result with negative images 4 hours after injection of 111In-pentetreotide (left) and a doubtful abdominal focus 24 hours after injection (right). Primary small bowel carcinoid was subsequently successfully resected. Copyright © 2006 by the Society of Nuclear Medicine.
|
On a per-patient basis, SRS was accurate in 15 of 19 tests with one FP and three FN (small lesion size; correspondence with FP on PET; unexplained elevation of urinary 5-HIAA levels). SRS was accurate in 10 of 14 noncarcinoid tumors.
"The main result of the present study was that 18F-FDOPA-PET appeared to be significantly more accurate in carcinoid tumors than in noncarcinoid tumors with an accuracy of 89% and 36%, respectively, on a per-patient basis," the authors stated.
Conversely, SRS proved superior in noncarcinoid tumors, especially for the detection of pancreatic tumors, they added.
They recommended that 18F-FDOPA-PET could be considered the first-line molecular imaging technique for the various segments of carcinoid tumors, from the primary tumor to staging, restaging, and occult recurrence.
By Shalmali Pal
AuntMinnie.com staff writer
September 14, 2006
Related Reading
Endoscopic capsules help pinpoint obscure GI bleeding, September 5, 2006
High homocysteine level linked to hip fractures in women, June 28, 2006
New promise for therapeutic radiopharmaceuticals, June 2, 2006
Copyright © 2006 AuntMinnie.com