Well, yes and no, the team concluded. The radiographers did fairly well, finding 100% of carcinomas and ensuring adequate colonic distension while there was time to correct it. On the other hand, a few too many missed lesions meant that the readers could not be recommended for solo fly throughs quite yet. They also had difficulty distinguishing true- from false-positive CAD marks.
Yet the talents of radiographers clearly have a role to play in screening in the U.K., and focused training with the CAD application could potentially improve their interaction with the technology, suggested Dr. David Burling from St. Mark's Hospital in London. The study was presented at this month's European Society of Gastrointestinal and Abdominal Radiology (ESGAR) meeting in Istanbul.
"The exciting thing about this is whether radiographers in the future might be able to look at large volumes of screening cases in a very efficient, cost-effective way," Burling told AuntMinnie.com in an interview. Burling, the lead investigator in the study, is a consultant gastrointestinal radiologist at St. Mark's.
In another study presented at the ESGAR meeting, fifth-year medical students were given a chance to read VC data with three CAD systems as backup. CAD helped significantly, but the students also had trouble ruling out CAD's false-positive detections.
Radiographers read VC
Radiographers are key members of the imaging team in the U.K.'s National Health Service, where an ongoing shortage of radiologists would leave radiology departments buried without their skillfully delivered services. But using radiographers as primary readers remains controversial, especially, it seems, in the view of non-U.K.-based physicians.
The aim of the St. Mark's study was to prospectively assess CAD-assisted radiographer performance in routine clinical practice. CAD as a second reader has yielded sensitivity as high as 96% in controlled studies, but experience in daily clinical practice has been limited, Burling said.
The investigators also sought to evaluate patient triage by management strategy, lesion detection accuracy, interpretation time, and the learning curve for new readers.
The study examined 304 symptomatic patients (119 men, 185 women; mean age 69 years) over a nine-month period. The researchers used a standard VC technique with both primary 2D and 3D interpretation that was randomly assigned, in addition to CAD as a second reader.
|
|
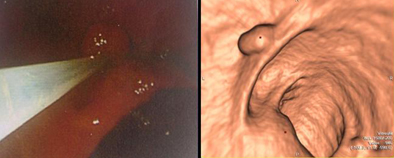
An 8-mm polyp in the ascending colon is seen at 3D VC (right) and at subsequent endoscopy (left).
|
Five radiographers underwent a standard VC training program that included a review article on virtual colonoscopy, an anatomy lecture, a hands-on training course, and a one-day VC workshop. Each radiographer completed 50 cases (mixed pathology) with feedback, and attended a one-hour session on the CAD scheme as well, and the lead radiographer had double-reported 104 additional VC exams prior to the study.
In all, 304 consecutive patients underwent VC as part of their routine clinical care. All had symptoms suggestive of an elevated risk of colon cancer. The patients underwent purgative bowel cleansing and colonic insufflation.
With the patient waiting onsite, a radiographer followed by the program coordinator read the data using a workstation (Vitrea 3.9, Vital Images, Minnetonka, MN) and CAD (ColonCAD, Medicsight, London).
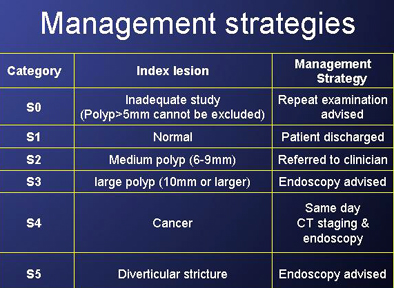
They documented all colonic neoplasia and interpretation times and proposed a patient management strategy code for each exam that was similar to the C-RADS system (S0-S5; see image below). Findings were compared to a reference standard consisting of expert radiologists' consensus findings, as well as clinical, surgical, and colonoscopic results when available.
|
|
Management codes S0-S5 were proposed for the index lesion in each case in a manner similar to C-RADS classifications.
|
The management strategies were then compared using Kappa, effect of 2D/3D analysis using Fisher's exact test, learning curve over time using logistic regression (strategy), and Pearson's correlation coefficient for reporting times, the team reported in an abstract.
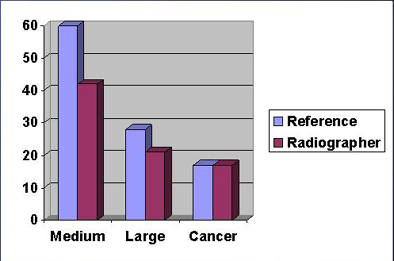
According to the results, 78 (26%) cases were abnormal, including 109 significant polyps or cancers. The CAD-assisted radiographers detected all of the cancers (17/17, 100%), 21 of 29 (72%) polyps 10 mm and larger, and 42 of 63 (67%) polyps ranging from 6 mm to 9 mm in diameter.
The results were in agreement with the S1 reference strategy in 187 of 211 (89%) examinations, with S2 in 19 of 28 (70%) exams, with S3 in 12 of 19 (63%) exams, and with S4 in 17 of 17 (100%) exams.
Overall agreement (S0-S5) was good between the readers (k = 0.72; confidence interval [CI]: 0.65-0.78). Moreover, no significant differences in strategy accuracy were found between primary 2D and 3D reads (p = 0.42) or over time (CI: 0.76-1.0; p = 0.12). The mean interpretation time with CAD was 17 minutes, decreasing over the study duration to 14 minutes over the last 50 exams. The correlation coefficient was -0.46 (p < 0.001).
|
|
There were 105 polyps/cancers in 78 exams. Radiographers (burgundy) detected all 17 cancers. Radiographers' detection performance lagged most behind the reference standard (lavender) in the detection of medium-sized polyps.
|
In analyzing the results, the authors said that while radiographers can provide a clinically useful initial interpretation for cancer triage and colonic distension, polyp detection and interpretation times do not currently support independent radiographer reporting.
While the radiographers detected 100% of the cancers, their sensitivity for the detection of clinically significant polyps 1 cm and larger fell short, at 72%. And compared to the reference standard, the nonradiologist readers lagged in accepting or rejecting positive CAD marks, though in this shortcoming, radiographers have traditionally had no shortage of company from their radiologist colleagues.
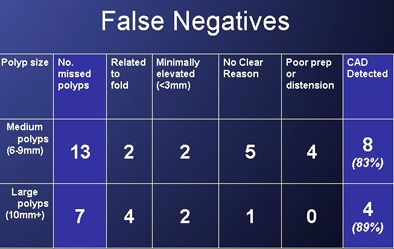
"CAD identified three polyps [1 cm or larger] that the radiographers chose to reject," Burling told AuntMinnie.com. Had they accepted all of the CAD annotations correctly, their detection rate would have been 83% and 89% for medium- and large-sized polyps, respectively.
|
|
Radiographers missed 13 of 63 medium-sized lesions and seven of 29 polyps 1 cm and larger, of which CAD detected eight and four, respectively.
|
"This raises a new question for the community as to whether there should be specific training packages on the use of CAD with CTC [CT colonography]," Burling said. "It might be that the incremental benefit of CAD could be improved by CAD-specific training and they could learn to accept or reject [CAD marks] better."
Potentially confounding the study results is the fact that all readers have different aptitudes and improve at varying rates with regard to experience and training, according to Burling. "I think training is an independent variable; I wonder if training on CAD specifically may also be an independent variable," he said.
But there's no doubt that radiographers are useful in CTC screening. Of significant importance, he said, radiographers are adept at detecting poor colonic distension from scout images and can ensure adequate distension prior to imaging.
Medical students get their chance
In another study presented at the ESGAR meeting, Dr. Zsolt Tarján and colleagues from Semmelweis University in Budapest, Hungary, recruited fifth-year medical students, pitting them against a radiologist experienced in VC in the interpretation of 50 colonoscopy-confirmed VC datasets. CAD was used as a second reader.
They employed five different reading strategies, including 2D reading, 2D reading with CAD prompts, 3D endoluminal reading, 3D reading with CAD prompts, and CAD read alone using an academic CAD system, according to the abstract.
For the detection of polyps and masses larger than 5 mm in diameter, the radiologist using CAD prompts achieved 93% sensitivity with 0.7 false-positive findings per case. This compared to 85%-89% sensitivity with 5.2-6.3 false positives per case for the medical students. CAD alone generated 87% sensitivity with 4.8 false positives per case (p > 0.05), the authors wrote.
Primary 2D reading was the fastest strategy, handled by the radiologist in 52 ± 34 seconds, and much more slowly by the medical students in 267 ± 123 seconds. Using the primary 3D read took significantly longer (p < 0.05) and yielded higher sensitivity but reduced specificity for all readers compared to 2D reading plus CAD.
"CAD prompts bring the sensitivity of medical students close to that of a skilled radiologist in reading CTC data, but the CAD or students with CAD could not rule out false positives effectively," Tarján and colleagues concluded.
By Eric Barnes
AuntMinnie.com staff writer
June 24, 2008
Related Reading
Gastroenterologist beats radiologist in dual-prep VC match, June 6, 2008
Radiographers equivalent to radiologists in VC study, March 19, 2007
VC CAD helps junior readers catch up, May 4, 2006
VC experts have an edge over less experienced readers, March 8, 2005
Training key to VC performance, but how much is anyone's guess, February 8, 2005
Copyright © 2008 AuntMinnie.com